MIPS & MACRA
Medicare in 2015 consolidated and streamlined various physician quality reporting systems and programs into the current Quality Payment Program (QPP) under the Merit-Based Incentive Payment System (MIPS) and Medicare Access and CHIP Reauthorization Act of 2015 (MACRA).
The QPP program focuses on improving the quality of care rendered to Medicare beneficiaries. The reimbursement structure under QPP is based on quality of care provided and not on the volume of patients seen by physicians. Physicians earn a performance-based payment adjustment to their reimbursement by Medicare. The payment will be based on the reporting of quality data to CMS using an electronic health record (EHR) system.
MIPS Components
- Quality: This replaces Physician Quality Reporting System (PQRS) program. This is 60% of the total quality measures reported.
- Cost: Replaces value-based modifier (VBM) program with no assigned value.
- Improvement Activities: This a new component added and accounts for 15% of quality measures reported.
- Advancing Care Information: Replaces the EHR Incentive Program or “Meaningful Use” and accounts for 25% of the quality measures reported.
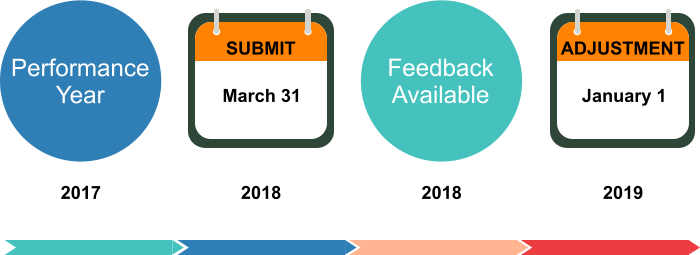
Implementation Timeline
BMI technology platform provides valuable opportunities for physicians who participates in the CCM program:
- Accelerate MIPS/MACRA Compliance: Physicians satisfy the mandated reporting requirements under the Merit-Based Incentive Payment System (MIPS) and
- Provides a HIPAA-compliant platform.
- Preparation for value-based care and risk-based contracts.
- Increased patient volume and maximize revenue opportunities with minimal investment.
How BMI Help Physicians and Practices
- Determine which MIPS applies to you
- Review available performance categories
- Select Your Quality Measures
- Review selected data
- Determine individual of group reporting scheme
- Select reporting mechanism
- Conduct Security Risk Analysis
- Report for at least 90 days
- Finalize MIPS performance requirements
- Submit MIPS data
Ready to participate in MIPS/MACRA? Call 201-428-9090 to speak with a Program Specialist

